Chaves P, Simoes D, Paco M, Pinho F, Duarte J, Ribeiro F. Cyriax’s deep friction massage application parameters: Evidence from a cross-sectional study with physiotherapists. Musculoskel Sci Pract. 2017;32:92-97.
Abstracted by: Elizabeth Sargent, PT, ScD, OCS, COMT, Burlington, VT – Fellowship Candidate, IAOM-US Fellowship Program & Jean-Michel Brismée, PT, ScD, IAOM-US Fellowship Program Director
Deep friction massage (DFM) for the treatment of tendinopathy has been used by physiotherapists for decades. Although anecdotal evidence exists to support its widespread use, scientific studies investigating DFM efficacy and effectiveness have reported variable results. A systematic review investigating DFM efficacy in the treatment of tendinopathy suggested that treatment parameters varied too widely for researchers to make any conclusions regarding treatment efficacy.1 The purpose of this study was to determine the prevalence of deep friction massage (DFM) used in clinical practice and to characterize the application parameters chosen by physiotherapists. The study was a cross-sectional, observational, analytical study based on a national web-based survey in Portugal. In order to improve our understanding of DFM treatment efficacy and effectiveness, determining how DFM is used in clinical practice would be helpful.
Methods: 478 physiotherapists completed an online questionnaire regarding the use of deep friction massage in clinical practice. The questionnaire, written by five physiotherapists, was emailed through lists provided by the Portuguese Association of Physiotherapists and through online social and professional networks. The questions fell into one of two categories: 1) personal characteristics (demographic and anthropometric) and professional profile (educational degree, years of clinical practice, professional context, dominant area of intervention, weekly workload and number of patients treated per day) and 2) DFM utilization. Physiotherapists provided information about the clinical conditions in which DFM was used and if the condition was a degenerative tendinopathy. In addition, information regarding application protocol was collected, such as frequency, tendon positioning (with or without tension), and criteria used to determine pressure applied to the affected area.
Results: Of the 478 participants, 421 (88%) reported the use of DFM in clinical practice. The conditions in which DFM was most frequently used were: 1) tendinopathy (n = 406; 84.9%), 2) muscle tear (n = 174; 36.4%), and 3) tenosynovitis (n = 160; 33.5%). Only 55.9% of physiotherapists reported the use of DFM for degenerative tendinopathy due to the perception of poor clinical outcomes and high patient stress. Regarding tendon position, similar numbers of participants performed DFM with or without stretching of the patellar tendon; whereas, the majority of participants performed DFM to the Achilles tendon with stretching and to the lateral epicondyle without stretching. Finally, parameters that participants reported to define and adjust the pressure used during DFM were presence of pain, tendon depth, injury acuity, type of injury, patient characteristics, tendon size and location.
The investigators characterized two clinical practice patterns among the study participants: 1) similar to Cyriax’s recommendations (high probability of performing DFM with the tendon in the correct position and for the correct duration) and 2) different from Cyriax’s recommendations (low probability of performing DFM with the tendon in the correct position and for the correct duration). A high number of participants who use DFM in clinical practice had a high probability of using the right treatment duration in acute conditions (80.2%), while a low number of participants used the correct treatment duration in chronic conditions (31.0%), regardless of practice pattern category. The mean duration of DFM application reported was 4 minutes for acute conditions and 5 minutes for chronic conditions. The primary difference between practice pattern category was related to tendon position during DFM. Participants with post-baccalaureate degrees (masters or PhD), more than 11 years of clinical experience, working 36-40 hours per week and seeing 3 or more patients per hour were more likely to perform DFM according to Cyriax’s recommendations.
IAOM Commentary: The IAOM was founded in 1978 by Dr. James Cyriax and Dos Winkel, a physical therapist, with the goal of providing continuing education opportunities for physicians and physical therapists seeking expertise in orthopedic medicine and manual therapy. Consequently, IAOM instructors have worked closely with Dr. Cyriax over the years learning the application parameters of DFM. Application recommendations according to Cyriax involve precisely locating the site of the lesion, moving subcutaneous fascia against underlying tendon, and moving transversely across affected fibers with sufficient depth and pressure.2,3 Initially, the DFM depth is determined by patient tolerance (mild pain is acceptable) and increased over the duration of each treatment.2 The recommended treatment duration for chronic tendinopathy according to Cyriax is 10-20 minutes until analgesia has been achieved and at an interval of every 48 hours.2
Similar to this study’s findings, the IAOM instructs physiotherapists to perform DFM to the lateral epicondyle without stretch (Figure 1) and to the Achilles tendon with stretch (Figure 2). Patellar tendon DFM is shown in Figure 3. The authors of this study report that the majority of studies involving DFM thus far do not provide sufficient detail regarding treatment duration and tendon position. Animal-model research has informed a paradigm shift of understanding tendon disease at a tissue level. Chronic tendinopathic tissue is disorganized and fibrous with increased type III collagen content.4 In addition, mechanical tendon stimulation has been shown to increase fibroblastic activity in rat tendon.5 Consequently, investigators are interested in examining the changes in tendon organization following the mechanical stimulation of DFM. Perhaps the lack of evidence supporting the use of DFM for treatment of tendinopathy is primarily due to the fact that investigators have failed to follow Cyriax’s treatment recommendations with regard to duration and tendon position. A common mistake among physiotherapists who use DFM in the treatment of chronic tendinopathy is insufficient treatment duration. Future research should investigate the effects of DFM on tendon morphology and histology following the recommended 10 to 20-minute application in chronic tendinopathy.

Figure 1. DFM to the lateral epicondyle at the extensor carpi radialis brevis (ECRB) insertion, the most common site of tendinopathy at the lateral epicondyle. The patient is sitting with the arm in 45o of shoulder abduction and 90o of elbow flexion. The therapist’s forearm is in line with the patient’s upper arm and s/he uses the tip of the thumb to sweep across the fibers.

Figure 2. DFM to the Achilles tendon. The patient’s foot is brought into dorsiflexion while the therapist grasps the most tender part of the tendon between the thumb and index finger and sweeps upward.
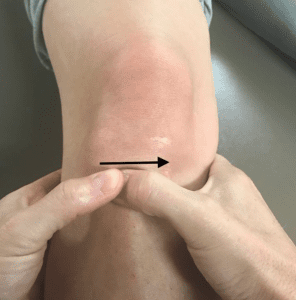
Figure 3. DFM to the patellar tendon. The therapist reinforces one thumb with the other and sweeps medially across the fibers.
- Joseph M, Taft K, Moskwa M, Denegar C. Deep friction massage to treat tendinopathy: A systematic review of a classic treatment in the face of a new paradigm of understanding. J Sports Rehabil. 2012;21(4):343-353.
- Stasinopoulos D, Johnson M. Cyriax physiotherapy for tennis elbow/lateral epicondylitis. Br J Sports Med. 2004;38(6):675-677.
- Chamberlain G. Cyriax’s friction massage: A review. J Orthop Sports Phys Ther. 1982; 4(1):16-22.
- Maffuli N, Ewen S, Waterston S, et al. Tenocytes from ruptured and tendinopathic Achilles tendons produce greater quantities of type III collagen than tenocytes from normal Achilles tendons: An in vitro model of human tendon healing. Am J Sports Med. 2000;28:499-505.
- Davidson C, Gehlsen G, Verhoestra B, et al. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sport Exerc. 1997;29:313-319.

