Järvinen T, Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Kalske J (2017). Arthroscopic Partial Meniscectomy vs Sham Surgery for Degenerative Meniscus Tear. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 30(6).
Article Summary by Jade McFarland, SPT from Missouri State University, Springfield, MO
Arthroscopic partial meniscectomy (APM) is one of the most common orthopedic operations, with an incidence that has increased steadily from 1990s until late 2010s. Many guidelines and expert opinions will allocate for surgery for a degenerative meniscus tear after there has been a failure of conservative treatment. The goal of this study was to assess if APM is superior to placebo-surgery in the treatment of patients with degenerative tear of the medial meniscus over the course of 24 months.
This study consisted of a multicenter, randomized, participant blinded and outcome assessor blinded, placebo-surgery controlled trail consisting of 146 adults with ages ranging from 35-65 years. There were 70 patients assigned to APM and 76 to placebo. On average, half of the participants in both groups reported mechanical symptoms of their knee preoperatively. There were 34 participants with a tear morphology defined as ‘unstable’ in the APM group, 41 in the surgery-placebo group. The participants had knee symptoms for over 3 months, consistent with medial meniscus tear and unresponsive to conventional conservative treatment with no clinical or radiographic knee osteoarthritis. Exclusions included obvious trauma-induced onset of symptoms or with a recent history of locked knee. Patients first underwent diagnostic knee arthroscopy and were then randomly assigned to APM or the placebo group.
During the APM, the damaged and loose bodies of the meniscus were removed, no other surgical procedure was performed. For the placebo surgery, APM was simulated to mimic the sensation and sounds of a true APM. With both the APM and placebo group, postoperative care was delivered according to a standardized protocol specifying that all participants receive the same walking aids and instructions for the same graduated home-based exercise program.
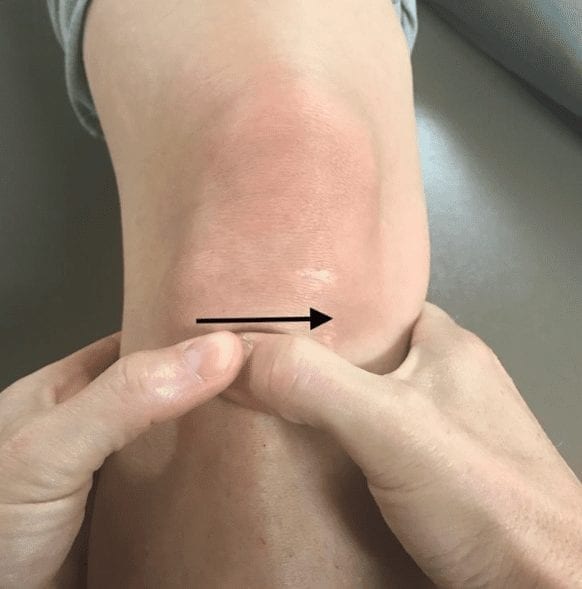
Testing was performed at baseline to 24 months after surgery. Participants were followed up by questionnaires at 2, 6, 12, and 24 months. At the 24-month follow-up, all participants were also clinically examined by an independent orthopedic surgeon unaware of the treatment allocation. Standardized clinical examination meniscal special tests were performed: McMurray test, pain provoked by joint line palpation and pain provoked by forced flexion and varus. Range of knee motion, knee crepitus, bony enlargement, effusion, location of pain at palpation and knee stability were also recorded. Primary outcome measures of this study included: Western Ontario Meniscal Evaluation Tool, the Lysholm knee score, and pain after exercise.
Results demonstrated a marked improvement in all primary outcomes for both groups. The difference between the groups did not reach statistical significance. Most of the participants in both groups were satisfied. No between-group difference was observed in the participants’ frequency in returning to normal activity level or frequency of mechanical symptoms. Overall, the authors found no statistically significant difference between the APM and placebo-surgery for symptomatic patients with degenerative meniscus tear and no osteoarthritis in any of the used outcomes measures over the course of 24 months. This study found no evidence to support that patients with the presence of mechanical symptoms or certain meniscal tear characteristics or those who had failed initial conservative treatment are more likely to benefit from APM.
PERSONAL COMMENTARY:
Surgical intervention is often allocated upon failure of conservative treatment. The above discovered no significant difference in outcomes between an APM and placebo-surgical groups. This raises the question whether surgery should continue to be recommended upon failure of initial conservative treatment for degenerative meniscal tear.
Of additional interest, it is important to recognize the biopsychosocial aspect when it comes to patient care and the importance of education and confidence. A recent systematic review was published by Louw et al and noted individuals with sham orthopedic surgery versus real orthopedic surgery both yielded similar findings regarding reducing pain and disability. Of further related interest, an article by Bialosky et al discussed the magnitude of a placebo intervention. The enthusiasm of the practitioner resulting in the more positive the patients’ beliefs and perception of the intervention, correlated with a positive outcome.
References:
Bialosky, J. E., Bishop, M. D., & Penza, C. W. (2017). Placebo Mechanisms of Manual Therapy: A Sheep in Wolfs Clothing? Journal of Orthopaedic & Sports Physical Therapy, 47(5), 301–304.
Louw, A., Diener, I., Fernández-De-Las-Peñas, C., & Puentedura, E. J. (2016). Sham Surgery in Orthopedics: A Systematic Review of the Literature. Pain Medicine.