Russell Hanks PT1
Valerie Phelps PT, ScD1,2
Jean-Michel Brismée PT, ScD2,3
1Advanced Physical Therapy Alaska, Anchorage, AK.
2International Academy of Orthopedic Medicine-US, Tucson, AZ.
3Texas Tech University Health Sciences Center, Center for Rehabilitation Research, Lubbock, TX.
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
Address correspondence to Russell Hanks, 1917 Abbott Rd., Suite 200, Anchorage, AK 99507. E-mail: rhanks@aptak.com
Abstract
While it is common for school aged children to experience low back pain (LBP), the need to seek medical consult is rare. Intrinsic causes of low back pain in children can include mechanical, developmental, infectious/inflammatory, and neoplastic. In young athletes, protrusion can be prevalent. This paper focuses on a case study of lumbar intervertebral disc (IVD) protrusion in a young athlete with atypical signs and symptoms of adult lumbar IVD herniation. This led to mis- and under-diagnosis and a long bout of unsuccessful conservative care. In hindsight, the patient presented with signs and symptoms characteristic of significant lumbar IVD protrusion in adolescents, particularly to a degree where surgery is indicated. Like many adolescent lumbar IVD herniations, this patient presented with neither leg pain nor neurological findings. He did, however, have two signs indicative of a massive intradiscal nucleus displacement: (1) the hip-waist extension stiffness phenomenon, also known as hamstring stiffness syndrome, and (2) a shuffling gait.
Background
Mechanical low back pain (LBP) is common in the pediatric population1 and approximately 35% of adolescents’ experience LBP at some point in their lives.2 Low back pain is now recognized to occur early in childhood and is associated with high prevalence rates of 22%2 and 51%3. Several studies have reported increased LBP after 12 years of age, particularly among girls.2,4,5,6 A statistically significant relationship was found between frequency of sports activities and spinal pain in children aged 7 to 17.7 Surgery for such cases is rare, with a recent study from Norway reporting that of 3,245 surgical patients, 97 patients (3%) were adolescents (between the ages of 13 and 19) while the remaining 3,148 were between the ages of 20 to 50 years.8
Intervertebral Disc (IVD)-related disorders are the direct result of “degenerative” changes in the lumbar IVD and 60% of all IVD pathology occurs in the lumbar spine.9 While IVD prolapses most commonly occur in middle aged patients, between the ages of 30 to 45, they can also be seen in children as young as 14 of either gender.10 Younger individuals with LBP are commonly afflicted with a IVD-related disorder where the “soul” of their symptoms resides in the acute mechanical and chemical changes in the IVD.11 Age appears to have a direct influence on the source of a patient’s LBP12 and the IVD begins to change at approximately 20 years of age.13 Thus, IVD protrusion and herniation in the adolescent are considered to have a genetic and/or traumatic origin.1,14,15 Although the main causes of adolescent low back pain are often mechanical, associated with lack of physical activity or strenuous exercise, diagnostic management is strongly recommended.16 In order to properly manage these patients, a clinician’s understanding of the pathoanatomy, physiology, and mechanics of the lumbar spine are foundational for clarity in differential diagnosis.
The severity of symptoms from juvenile lumbar IVD protrusion or prolapse are not always dependent on the size of the protrusion or prolapse and are believed to be due to irritation of the posterior longitudinal ligament and the dura mater. The absence of severe symptoms is frequently observed in children and adolescents with an IVD prolapse, often only complaining of a stiff back and a “pulling” feeling in the back and/or one or both legs.12,17
The posterior longitudinal ligament (PLL) does not provide an appreciable biomechanical constraint to movement.11 Its deeper fibers merge with the outer annulus and can produce nonradicular pain when irritated with an IVD protrusion or prolapse due to the multi-segmental innervation by the sinuvertebral nerve.18 The PLL is consistently connected to the dura mater at the lower lumbar disc levels through Hofmann ligaments and dense fibrous adhesions.19,20,21 The pain produced by a IVD protrusion is partially related to the disruption of these adhesions through branches of the sinuvertebral nerve resulting in a positive straight leg raise (SLR) without any appreciable radiological bulge representing an external disc disruption, especially in young patients with an extension trauma.11
Despite the outer annulus IVD strength, it is still vulnerable to injury. Younger individuals involved in sports are often at risk for external IVD disruptions. They often present with sagittal plane (flexion and extension) movement limitations due to the tension or compression forces across the outer annulus.22,23,24 Often the pain is local, provoked with slump or SLR testing with distal initiation through dorsiflexion of the ankle and knee extension, which tension loads the outer annulus through the root and ligaments of Hofmann.11 Usually these symptoms are self-limiting with generalized activity and limiting painful provoking movements.
While it is common for school aged children to experience LBP, the need to seek medical consult is rare.14 This paper focuses on a case study of diagnosed lumbar IVD protrusion in a young athlete with atypical signs and symptoms of adult lumbar IVD herniation. This led to mis- and under-diagnosed condition resulting in a long bout of unsuccessful conservative care. In hindsight, the patient presented with signs and symptoms characteristic of lumbar IVD protrusion in adolescents, particularly to a degree where surgery was indicated. Like many adolescent lumbar IVD herniations, this patient presented with neither leg pain nor neurological findings. He did, however, have two signs that were indicative of massive intradiscal nucleus displacement: (1) the hip-waist extension stiffness phenomenon, also known as hamstring stiffness syndrome; and (2) a shuffling gait.12,25,26
Case Report
A 16-year old male was referred to physical therapy for evaluation and treatment of LBP; he was a track and football athlete. He described a 4-month history of LBP, rated 7/10 on the visual analog scale, that had been aggravated since the previous track season while performing warm-up stretches and subsequently increased after performing deadlifts during weight training at school. He reported increased pain after activity and managed most of his symptoms with non-steriodal antiinflammatory drugs (NSAIDs), although it provided only minimal pain relief. At the initial visit, he had undergone no imaging of his spine or pelvis.
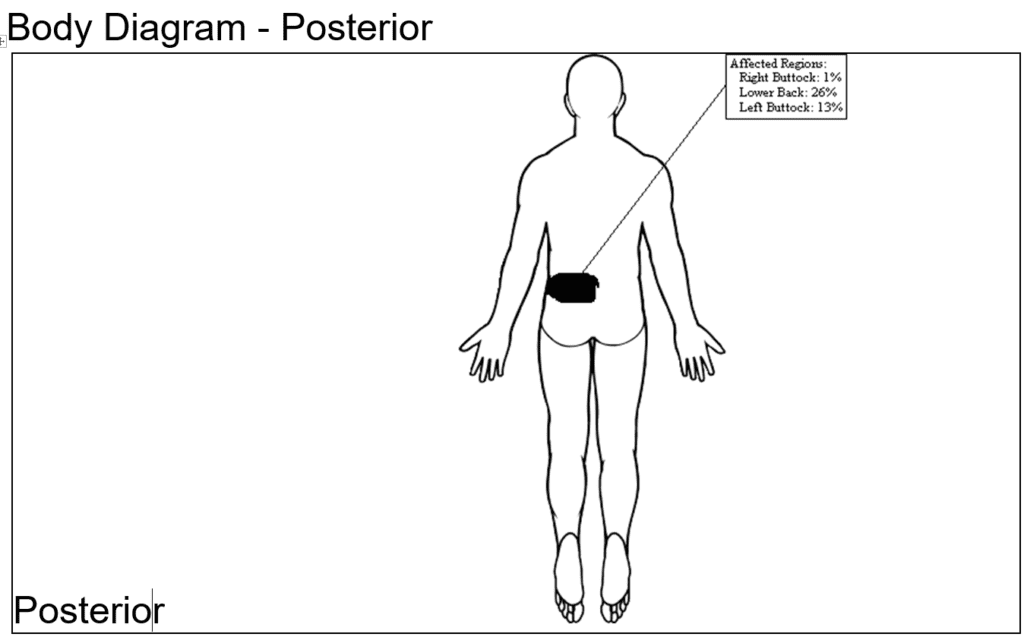
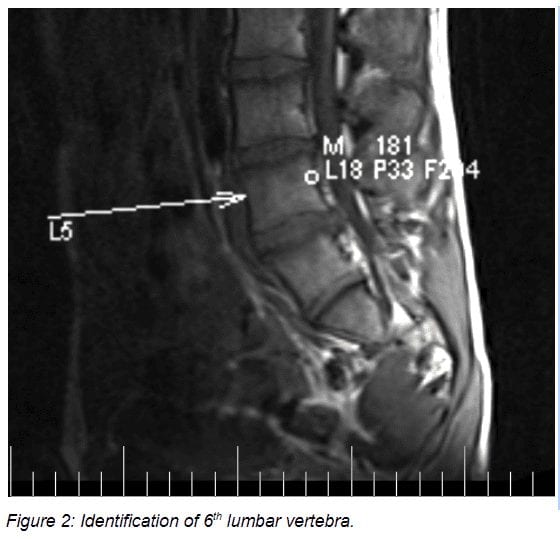
Figure 1: Pain complaints
The patient’s chief complaints were of localized pain in the upper inner quadrant of the buttock. (Figure 1) The symptoms were primarily on the left, and he felt that he had to sustain a constant contraction of his lumbar and leg muscles to keep from experiencing the same pain (to a lesser degree) on the right. He reported constant pain and was unable to find a position of comfort.
See Table 1 for Basic Clinical Examination findings at the initial visit and again at 6 months following diagnostic injection.
Table 1 – Clinical Examination
| POSITION
TEST |
FINDINGS – Initial | FINDINGS – at 6 months
Post diagnostic injection evaluation to determine lumbar involvement versus sacroiliac joint (SIJ) and gluteal region |
| Standing
Observation |
Right lateral shift and forward bent | Patient walked in a stooped manner, without arm swing, and with slightly flexed hip and knee joints. Severely deviated standing posture: forward bent and right lateral trunk shift. |
| Forward flexion | 75% limitation, moderate pain | 60% limitation, moderate pain |
| Forward Flexion with cervical flexion | Increased intensity of pain | Increased to severe pain |
| Extension | 75% limitation, moderate pain | 100% limitation, severe pain |
| Left Sidebending | 25% limitation, moderate pain | Within normal limits (WNL), no change in pain |
| Right Sidebending | 25% limitation, moderate pain | WNL, no change in pain |
| Strength Tests in Standing
Heel walk & unilateral toe raises |
Strong/painless | Strong/painless |
| Neural Tests in Sitting
Slump test left distal initiation |
Slight pain increase with cervical flexion and moderate increase with left ankle dorsiflexion (DF), knee ext. | Severe pain at the left upper inner quadrant of the buttock with increased pain on ankle DF, no change with cervical flexion |
| Slump test right distal initiation | negative | Moderate pain at the left upper inner quadrant of the buttock with increased pain on ankle DF, and increased intensity with cervical flexion |
| Passive Motions Supine
Hip flexion Left |
120° range of motion (ROM) | 95° with moderate pain at the upper inner quadrant of the left buttock |
| Hip flexion Right | 120° ROM | 100° ROM |
| Hip internal rotation: Left | 45° ROM | 45° ROM with minimal pain at the upper inner quadrant |
| Hip internal rotation: Right | 45° ROM | 45° ROM |
| Hip external rotation: Left | 40° ROM | 45° ROM with severe pain at the upper inner quadrant and apprehension |
| Hip external rotation: Right | 40° ROM | 45° ROM |
| SIJ provocation: dorsolateral | negative | Negative, but very mild pain with Gaenslen and thigh thrust |
| Neural Tests Supine
Straight Leg Raise: Left |
Increased pain with cervical flexion and left ankle (DF) | Hip-waist extension stiffness phenomenon* |
| Straight Leg Raise: Right | Negative | |
| Resisted Testing: Supine & Prone
All resisted motions testing myotomes L1 to S2) |
Normal strength | Normal strength |
| Neural Tests Sidelying
Femoral nerve stretch left |
Negative | Hip extension loss of 10 degrees to neutral |
| Femoral nerve stretch right | Negative | Hip extension loss of 10 degrees to neutral |
| Reflex Testing:
Patellar & Achilles Reflexes |
No response | No response |
| Babinski (Foot sole reflex) | No response | No response |
| Sensory Testing:
Light touch: Left & Right |
Normal | Normal |
| Prone
Spring Testing |
2/10 pain L3, 5/10 pain L4 and L5 | Moderate pain at L4 and L5 |
* Hip-waist extension stiffness phenomenon, also known as hamstring stiffness syndrome,26 is seen in the most extreme form of adolescent IVD protrusion or prolapse. In such cases, during the SLR test, the other leg and the entire back move immediately with the tested leg. These children walk with a shuffling gait, whereby the hip and knee joints are slightly flexed.12,17
Plan of Care
Based on the initial findings in this case, the diagnosis was lumbar IVD pain. Examination testing supporting this diagnosis were the painful and limited lumbar sagittal movements, increased dural tension with left slump testing and positive straight leg raise. His deviated posture also supported a discogenic diagnosis.
The patient was treated for 2 weeks for a total of 7 visits. Treatment emphasized soft tissue mobilization to the hips followed by joint specific treatment for direct hip mobilization emphasizing the improvement of extension. He also underwent static pelvic traction in a 90/90 position with half of his body weight for 20 minutes. He was instructed on core lumbar stabilization training with emphasis on transverse abdominal activation with application to function and ADL’s. He had 4 chiropractic adjustments in the week following his last physical therapy visit.
The high school football season was beginning in August and he decided to hold on his treatments to allow him to support the team on the sidelines during practices and games. His pain restricted him from playing. Treatment resumed in September; his symptoms were still local and severe, and 2 epidural steroid injections had failed to give him pain improvement. Additionally, he consulted with two local spine surgeons who determined he was not a candidate for surgery (lack of leg pain, and no neurological deficit could be found). He continued to undergo injections for pain management, and he consulted an orthopedic surgeon who diagnosed a gluteus medius tear and recommended surgical repair. Conservative therapeutic intervention had involved therapeutic ultrasound to improve tissue perfusion and reduce pain and selective training and skills-based practice to improve postural control strategies, spinal stability, balance, and/or coordination for restoration of functional mobility.
By January of the following year, symptoms had progressively worsened, and the patient was becoming withdrawn and angry as noted in school and around his friends. Symptoms were becoming more difficult to evaluate due to the pain levels, and thus, the proper treatment was difficult to identify; he was not responding to any form of treatment.
At this point, in consultation with the pain management physician, it was decided to collaborate in one final attempt to diagnose the pain generator. There was suspicion of sacroiliac joint (SIJ) arthropathy (as this is where the pain was isolated, and it was theorized that the SIJ problem would have interfered with gait), gluteal tear and/or superior gluteal neuritis, or lumbar IVD protrusion. Collaboration was strategized as follows: the patient would undergo an SIJ block, superior gluteal nerve block, and gluteal injection, all with local anesthetic, after which he would undergo clinical assessment by the physical therapists.
Interpretation of Clinical Examination Findings and Diagnosis at the January visit:
The clinical examination following the SIJ and gluteal injection had the following findings: (1) See Table 1 for the Clinical Examination findings; (2) Hip abductor testing: mildly painful resisted abduction/ER (clam shell) with weak active hip abduction in sidelying with straight leg; (3) Tenderness to palpation of the superior gluteal nerve prior to injection with minimal to no pain after injection; and (4) Severe tenderness to palpation of the S2-3 junction on the left, and not at any other sacral level.
Signs and symptoms at the January testing clearly identified severe IVD pathology in the absence of leg pain or neurological deficit. The additional signs of shuffling gait and hamstring stiffness syndrome, along with the 6 months of failed conservative care, made it clear that surgery was the only way to obtain relief for this young man. The mild SIJ provocation testing and the gluteal muscle testing was considered secondary to the IVD pathology and it was determined that consult with a pediatric spine surgeon would be the next best step.
Magnetic Resonance Imaging (MRI) Imaging was available at the January visit and demonstrated prominent protrusions at two levels. See Figures 2 to 4


Subsequent Care:
The physical therapists and pain physician helped the parents identify an appropriate pediatric surgeon at a well-known medical center in a large metropolitan area. A consult was obtained within 2 weeks. The surgeon requested a 6-week trial of 15 mg. oral Meloxicam. This brought no change in symptoms and laminotomy and microdiscectomy on left L5-L6 and right L6-S1 surgery was performed in March 2015.
Follow Up:
Within 3 months following surgery, the young male had returned to track and field sports. At one year follow up to surgery, his Oswestry Disability Index U.2.1 had a total score of 0%. He did not receive follow up care in physical therapy, so it was not determined whether the stiffness in the trunk and hips remained. Several authors report that ongoing stiffness following surgery can be seen.12,17,26 At two years post-surgery, he secured a track and field walk-on position his sophomore year at a Division 1 Pac 12 university.
Discussion:
Low back pain should elicit an appropriate work-up because a serious underlying pathological cause can be found in cases of low back pain in children and adolescents’.14,16,27,28,29 Common specific diagnoses of a mechanical origin with IVD lesions or herniations should be listed as possibilities.14,30 Symptoms are often relieved by rest or reduction of physical activity and pain is enhanced with increased spinal load.31,32
There were many important findings in this case that can be specific to adolescent IVD protrusion. Because of the relatively late ossification of the growth centers of the vertebral body, manipulation (particularly rotatory manipulation) are not recommended as they could lead to apophyseal avulsion and/or a worsening of the IVD protrusion.12,33 What was particularly interesting about this case was an absence of leg symptoms, pain was very localized, and there were no neurological findings, which became a distractor for many of the clinicians treating this young patient. He had been diagnosed as having a gluteus medius tear by an orthopedic surgeon and SIJ arthropathy by a pain management physician. For instance, a recent study by Linkoaho et al15 (2017) included 89 patients, of which 19 underwent surgery. Every patient that underwent surgery had limb pain in contrast to the groups treated conservatively in which only 11 of 64 patients had limb pain. Clinical reasoning would follow that if an adolescent IVD herniation is severe enough to require surgery, significant limb pain would be a symptom.
Conservative care, which would be expected to be successful in a younger individual, had no effect. Interestingly, Linkoaho et al15 (2017) reported ‘Compared with adult disc herniation, conservative treatment in adolescents does not lead to resolution of pain as reliably as in adults,’ which was clearly the experience in this case. Variable symptoms in adolescent IVD herniation as well as lack of awareness of lumbar IVD herniation in adolescents may have consequences with prolonged pain that could adversely impact the outcome of surgical intervention.34,35 As a result, it can be a long time to diagnose, and gait abnormalities are often present.17,36 Children walk with a shuffling gait, whereby the hip and knee joints are slightly flexed. “Waddling gait with flexed knees is considered as pathognomonic for this condition and may be masked by the signs of root irritation due to prolapsed intervertebral disc material.”17
Additionally, unique to this case was the hamstring stiffness syndrome or hip-waist extension stiffness phenomenon that is seen in the most extreme form of adolescent IVD protrusion or prolapse. In such cases, during the SLR test, the other leg and the entire back move immediately with the tested leg. Orthopedic literature describes that the extreme stiffness can remain even after surgery.12,26 Lastly, the psychosocial impact on a youngster with undiagnosed and potentially undertreated lumbar IVD herniation can be devastating; this young man was observed over a year’s time to become more angry displaying emotional outbursts, withdrawn from friends and family, with increasing lack of self-confidence.37
Conclusion
There is ongoing debate regarding surgery for IVD herniation in adults in the absence of neurological deficit. Treatment of adolescents with herniated IVD is less clear.38
Herniated lumbar IVD problems in adolescents can have uncommon signs and symptoms. This case presented with localized buttock pain and no neurological deficits. Two pathognomonic signs were evident, however, and they are exclusive to adolescent lumbar pathology: (1) the hamstring stiffness syndrome (also known as the hip-waist extension stiffness phenomenon, and (2) the shuffling gait. There are less than a handful of articles describing similar findings, indicating the likelihood that this clinical phenomenon is not well known. It would behoove clinicians to be aware of the less common signs and symptoms of significant IVD pathology in adolescents to prevent long periods of unsuccessful treatment with increasing psychopathology. Surgery is generally recommended after 6 to 8 weeks of no improvement in conservative care in these cases.8,12,26
References
- MacDonald J, Stuart E, Rodenberg R. Musculoskeletal Low Back Pain in School-aged Children: A Review. JAMA Pediatr. 2017 1;171(3):280-287.
- Olsen TD, Andrews RL, Dearwater SR, Kriska AM, Cauley JL, Aaron DJ, LaPorte RE. The epidemiology of low back pain in an adolescent population. Am J Public Health 1992;82(4):606–608.
- Harreby M, Nygaard B, Jessen T, Larsen E, Storr-Paulsen A. Risk factors K.D. Watson et al. / Pain 97 (2002) 87–92 91 for low back pain in a cohort of 1389 Danish school children: an epidemiologic study. Eur Spine J 1999; 8:444–450.
- Troussier, B., Davoine, P., de Gaudemaris, R., Phelip, X., 1994. Back pain in school children—a study among 1178 pupils. Scand J Rehabil Med. 26, 143–146.
- Mierau D, Cassidy JD, Yong-Hing K. LBP and straight leg raising in children and adolescents. Spine. 1989 14, 526–528.
- Burton, A.K., Clark, R.D., McClune, T.D., Tilotson, K.M., The natural history of LBP in adolescents. Spine. 1996; 21, 2323–23.
- Balague´ F, Dutoit, G, Waldburger, M, 1988. LBP in school children: an epidemiological study. Scand. J. Rehabil. Med. 20, 175–179.
- Gulati S, Madsbu MA, Solberg TK, Sørlie A, Giannadakis C, Skram MK, Nygaard ØP, Jakola AS. Lumbar microdiscectomy for sciatica in adolescents: a multicentre observational registry-based study. Acta Neurochir (Wien). 2017 159(3):509-516.
- Kramer J. Bandscheibendedingte Erkrankungen. Stuttgart: Georg Thieme Verlag; 1978.
- Ali A, Khan SA et al. Lumbar disc herniation in patients with chronic backache. J Ayub Med Coll Abbottabad 2013; 25:68-70.
- Sizer P et al. Pain Generators of the Lumbar Spine. Pain Practice 2001; 3:255-273.
- Winkel D, Aufdemkampe G, Matthijs O, Meijer OG, Phelps V. Diagnosis and Treatment of the Spine: Nonoperative Orthopaedic Medicine and Manual Therapy. Gaithersburg, Co: Aspen Publishers, Inc; 1997.
- Nerlich AG, Schleicher ED, Boos N. Immunohistologic markers for age-related changes of human lumbar intervertebral discs. Spine. 1997; 22:2781-2795.
- Faingold R, Saigal G, Azouz EM, Morales A, Albuquerque PA. Imaging of low back pain in children and adolescents. Semin Ultrasound CT MR. 2004 25(6):490-505.
- Linkoaho O, Kivisaari R, Ahonen M. Spinal canal dimensions affect outcome of adolescent disc herniation. J Child Orthop 2017; 11:380-386.
- Boćkowski L1, Sobaniec W, Kułak W, Smigielska-Kuzia J, Sendrowski K, Roszkowska M. Low back pain in school-age children: risk factors, clinical features and diagnostic management. Adv Med Sci. 2007;52 Suppl 1:221-3.
- Atalay A, Akbay A, Atalay B, Akalan N. Lumbar disc herniation and tight hamstrings syndrome in adolescence. Childs Nerv Syst. 2003 Feb;19(2):82-5.
- Bogduk N. Clinical Anatomy of the Lumbar Spine and Sacrum. New York, NY: Churchill Livingstone; 2012; pages 405-409.
- Wadhwani S, Loughenbury P, Soames R. The anterior dural (Hofmann) ligaments. Spine. 2004; 29:623-627.
- Spencer DL, Irwin GS, Miller JAA. Anatomy and significance of fixation of the lumbosacral nerve roots in sciatica. Spine.1983; 8:672-679.
- Parke WW, Watanabe R. Adhesions of the ventral lumbar dura. Spine. 1990; 15:300-303.
- Harada Y, Nakahara S. A pathologic study of lumbar disc herniation in the elderly. Spine. 1989; 14:1020-1024.
- van der Windt DA, Simons E, Riphagen II, Ammendolia C, Verhagen AP, Laslett M, Devillé W, Deyo RA, Bouter LM, de Vet HC, Aertgeerts B. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev. 2010 17;(2):CD007431.
- Ekedahl KH, Jönsson B, Frobell R. Validity of the fingertip-to-floor test and straight leg raising test in patients with acute and subacute low back pain: A comparison by sex and radicular pain. Arch Phys Med Rehabil. 2010; 91:1243-1247.
- Kayser R1, Mahlfeld K, Heyde CE, Grasshoff H, Mellerowicz H. Tight hamstring syndrome and extra- or intraspinal diseases in childhood: a multicenter study. Eur Spine J. 2006 15(4):403-8.
- Zhu Q, Gu R, Yang X, Lin Y, Gao Z, Tanaka Y. Adolescent lumbar disc herniation and hamstring tightness: review of 16 cases. Spine (Phila Pa 1976). 2006 15;31(16):1810-4.
- Bunnell WP., Back Pain in Children. Orthopedic Clinics of North America. 1982; 13:587-604.
- Smith MS, Psychosomatic Symptoms in Adolescence. Medical Clinics of North America. 1980;74: 1121-1134.
- King HA., Evaluating the Child with Back Pain. Ped Clinics of N Am 1986; 33:1489-1493.
- Turner PG, Green JH & Galasko CSB., Back Pain in Childhood. Spine. 1989; 14:812-814.
- Balague F, Nordin M. Back Pain in Children and Teenagers. Bailliere’s Clinical Rheumatology. 1992; 6:575-593.
- Patel D, Kinsella E. Evaluation and management of lower back pain in young athletes. Transl Pediatr. 2017; 6:225-235.
- Zhao P, Feng TY. Protruded lumbar intervertebral nucleus pulposus in a 12-year-old girl who recovered after nonsurgical treatment: a follow-up case report. J Manipulative Physiol Ther. 1997 Oct;20(8):551-6.
- Silverplats K, Lind B, Zoëga B, et al. Clinical factors of importance after lumbar disc herniation surgery: long term follow-up. Eur Spine J. 2010; 19:1459-1467.
- Ng LCL, Sell P. Predictive value of the duration of sciatica for lumbar discectomy. J Bone Joint Surg [Br] 2004;86-B:546-549.
- Smorgick Y1, Floman Y, Millgram MA, Anekstein Y, Pekarsky I, Mirovsky Y. Mid- to long-term outcome of disc excision in adolescent disc herniation. Spine J. 2006;6(4):380-4.
- Engel-Yeger B, Keren A, Berkovich Y, Sarfaty E, Merom L. The role of physical status versus mental status in predicting the quality of life of patients with lumbar disk herniation. Disabil Rehabil. 2016 20:1-7.
- Fakouri B, Nnadi C, Boszczyk B, Kunsky A, Cacciola F. When is the appropriate time for surgical intervention of the herniated lumbar disc in the adolescent? J Clin Neurosci. 2009 16(9):1153-6.