Reference: Feldbrugge CM, Pathoomvanh MM, Powden CJ, Hoch MC. Joint mobilization and static stretching for individuals with chronic ankle instability: A pilot study. J Bodyw Mov Ther. 2019; 23(1): 194-201.
Abstracted by: Ryan Lasley PT, MPT, AT/L, COMT, NASM-CES/PES, Phoenix, AZ – Fellowship Candidate, IAOM-US Fellowship Program & Jean-Michel Brismée, PT, ScD, Fellowship Director, IAOM-US Fellowship program.
Context: Ankle sprains are prevalent in society and can be simple or complex in severity. Often ankle sprains evolve into chronic ankle instability (CAI) with long lasting negative effects on ankle range of motion (ROM), function, and quality of life. Numerous studies have touted both calf stretching and manual therapy as ways to improve on all limitations and impairments. Further research is needed to determine if one or both interventions are necessary for positive improvement. There is also a need to investigate the amount of time in which these interventions should be utilized in order to experience the positive gains desired.
Objective: The main focus of this study was to research the effect of talocrural joint dorsal mobilization and static calf stretching on dorsiflexion range of motion (DROM), health related quality of life reports (HRQL), and static and dynamic postural control via the star reach task.
Design: A randomized, non-control group, two-group pretest-posttest design.
Setting: A large public university.
Patients or Other Participants: Ten subjects (5 men, 5 women) voluntarily presented for the study. Demographic information included age of 24.4 ± 4.7years, height 172.1 ± 11.3 cm and weight 76.2 ± 17.1 kg.
Intervention(s): Static calf stretching was utilized daily for 4 weeks to address the soleus and gastrocnemius muscles. These stretches were performed once daily via a descriptive home exercise program (HEP) with the parameters 3 x 30 seconds hold for each stretch. Ankle talocrural anterior-posterior (AP) joint mobilizations were performed over the same 4-week period with either early implementation (first 2 weeks) or late implementation (last 2 weeks). First a 1-minute session of talocrural joint traction was applied to each ankle. Second, four 2-minute sessions of Maitland (grade III) AP joint mobilizations were performed. Between each set of Maitland AP mobilizations there was a 1-minute rest break.
Main Outcome Measure(s): Patient reported outcome (PRO) measures included the Disablement in the Physically Active Scale (DPA), Foot and Ankle Ability Measure (FAAM) Activities of Daily Living (FAAM-ADL) and Sport (FAAM-Sport) subscales, and the Fear Avoidance Belief Questionnaire (FABQ). DROM was measured using weight-bearing lunge technique (WBLT), in which the patient was placed into a lunge position with the patella touching the wall. The participants foot was moved posterior, away from the wall, in 1cm increments until the patella could not be maintained on the wall while the same heel sustained contact with the floor. Single-limb stance with eyes open and closed was used to assess static postural control while standing on a force plate for 10-seconds. The static postural control measure focused on Time To Boundary (TTB) calculations, which are based off of changes in participants’ foot Center of Pressure (COP) values while standing on the force plate. TTB values are basically changes in foot COP force values that are then broken down into sagittal and frontal plane vectors. These are used to help quantify a participant’s baseline, pre-intervention, and post-intervention balance capabilities. The researchers also calculated the means and standard deviations for the anterior-posterior and medial-lateral directions with the TTB calculations. Lastly, the star excursion balance test (SEBT-AR) was used to measure dynamic postural control. During this test the participants performed four practice trials and then three analysis trials in which reach distance was measured in centimeters and normalized to the participants leg length.
Results: There was no findings between the early- and late-mobilization groups at the end of this study. The WBLT score did demonstrate a significant improvement at post-intervention (baseline: 9.80 ± 4.16 cm, pre-intervention: 9.80 ± 3.60 cm, post-intervention: 11.20 ± 3.05 cm). The patient reported outcome measures FAAM-ADL (baseline – 88.45 ± 8.10, pre-intervention – 89.64 ± 5.59, post-intervention – 93.69 ± 5.24), DPA (baseline – 14.50 ± 9.57, pre-intervention – 16.00 ± 6.99, post-intervention – 11.80 ± 4.66), and FABQ-PA (baseline: 10.50 ± 2.55, pre-intervention: 10.4 ± 4.50, post-intervention: 7.7 ± 4.14) scores significantly improved at post-intervention. In the case of static and dynamic postural control, no significant differences were found in the post-intervention groups or between the early- and late-mobilization groups.
Conclusions: Patient’s experiencing chronic ankle instability (CAI) were found to experience significant improvement in self-reported ankle function, global well-being, and fear of re-injury when measured through numerous patient-reported outcome measures including the FAAM-ADL, DPA, and FABQ-PA. Significant improvement was also noted with ankle ROM from baseline measurements to post-intervention measurements regardless of the manual therapy intervention timing.
Clinical Impression: Patients following acute untreated ankle sprains may or may not eventually regain complete function.1 These types of patients may eventually develop CAI with a reduction in osteokinematic and arthrokinematic motion at the talocrural joint along with a reduction in neuromotor control with both static and dynamic balance activities. This reviewed article highlights the fact that rehabilitating the CAI patient is a complex endeavor. The use of manual therapy is effective at improving motion and self-reported quality of life and function as is seen through the WBLT and FAAM-ADL, DPA, and FABQ-PA, however neuromotor control was not positively impacted in this study. This contradicts other research that reported marked improvement in neuromotor control with the performance of single leg balance training in those with CAI.2 Consumers of this research article should make it a point to implement manual therapy into their treatment protocols with the purpose of improved osteokinematic and arthrokinematic motion only with no positive effect on neuromotor control.
Consistency of the Content: This article elaborates on the positive effect that manual therapy has on both osteokinematic and arthrokinematic motion when delivered to the talocrural joint by a licensed professional. This type of information is commonly taught in physical therapy curriculum along with continuing education courses and seminars. The article makes an interesting point that manual therapy alone is not enough to generate positive neuromotor control changes. The implementation of neuromotor control exercises is necessary to see positive static and dynamic postural control responses in patients experiencing CAI. This too, is consistent with physical therapy teachings.
References:
- Anandacoomarasamy A., Barnsley L. Long term outcomes of inversion ankle injuries. Br. J. Sports Med. 2005; 39(3): e14.
- Hale SA, Hertel J, Olmsted-Kramer LC. The effect of a 4-week comprehensive rehabilitation program on postural control and lower extremity function in individuals with chronic ankle instability. J. Orthop. Sports Phys. Ther. 2007; 37(6): 303e311.
Talocrural Joint Manual Physical Therapy Interventions

1a – To perform talocrural joint resting position traction the patient should be belted down to stop caudal tibial motion with the caudal pull of the talus and ankle. The patient has a towel placed dorsal to the popliteal fossa to generate 10° of knee flexion to reorient the tibial plafond to a vertical position since it has a 10° declination angle. The belt is looped around the middle ½ of the distal lower extremity and then fed cranial and belted under the plinth to maintain the required stabilization of the extremity. Please refer to Figure 1a-b.

1b

Figure 2a.
To perform resting position talocrural joint traction the treating therapist stands caudal to the patient’s affected foot while facing cranial. The therapist wraps his/her hand over the dorsum of the foot while aligning his/her 5th digits over the dorsal and proximal talus. The patient’s ankle is maintained in 10° of plantarflexion the entirety of the mobilization. The therapist pulls the talus and ankle in a caudal direction through the plantar aspect of the patient’s foot.

If the therapist wants to improve on ankle dorsiflexion the therapist can perform prepositioned axial separation into dorsiflexion. This is done first by the therapist aligning his/her hands as was described in Figure 2a. The therapist then places his/her thumbs under the plantar surface of the 1st and 5th metatarsals. The therapist performs the resting position talocrural joint traction and then adds a slight dorsiflexion spin action to the ankle by performing a scooping mechanism to the patient’s foot and ankle in a cranial direction. Please refer to Figure 2b.

Figure 3a.
To perform ventral 🡪 dorsal directed talocrural joint mobilizations to improve talocrural joint dorsiflexion the patient must have his/her proximal tibia stabilized. The belt is looped around the proximal tibia and belted under the plinth. Once again there is a towel placed dorsal to the popliteal fossa to allow for 10° of knee flexion and to align the tibial plafond into a vertical position. Please refer to Figure 3a – b above and below.

3b
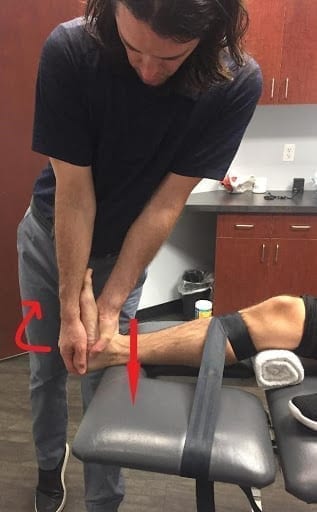
Figure 4a.
To perform ventral 🡪 dorsal directed talocrural joint mobilizations to improve talocrural joint dorsiflexion the therapist first primes the joint by mobilizing it from a resting position of 10° of plantarflexion. The therapist stands lateral to the patient with his/her distal hand stabilizing the plantar foot and calcaneus in the 10° of plantarflexion necessary. The treating therapist places the webspace between the 1st and 2nd phalanx over the patient’s ventral talus while maintaining a forearm supinated position. The therapist delivers a ventral 🡪 dorsal directed force to the talus through the hand placed over the ventral talus. Please refer to Figure 4a.
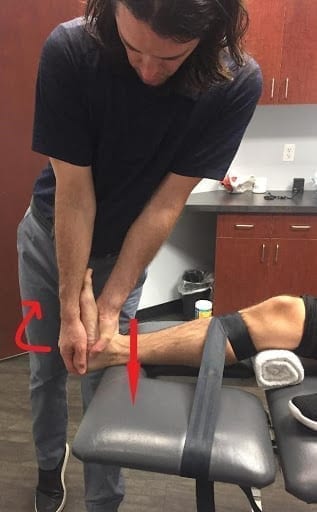
Figure 4b.
To perform ventral 🡪 dorsal directed talocrural joint mobilizations to improve talocrural joint dorsiflexion the therapist can preposition the talocrural joint into a dorsiflexion position that is different than the previously mentioned position of 10° plantarflexion. The therapist continues to stand lateral to the patient with his/her distal hand stabilizing the plantar foot and calcaneus. The therapist then uses this hand to preposition the foot/ankle into his/her dorsiflexion movement limitation by spinning the talocrural joint in the dorsiflexion direction. The treating therapist maintains the webspace between the 1st and 2nd phalanx over the patient’s ventral talus while also maintaining a forearm supinated position. The therapist then delivers a ventral 🡪 dorsal directed force to the talus through the hand placed over the ventral talus. Please refer to Figure 4b.

Figure 5a.
To improve talocrural joint dorsiflexion in the closed chain the patient is placed into a stride-standing position on an elevated plinth with the patient maintaining his/her balance by holding a dowel rod. The OPTP manual wedge if placed at the medial calcaneus to maintain a subtalar neutral position. Please refer to Figure 5a – b.

5b

Figure 6a.
In order to improve ankle dorsiflexion in the closed chain the patient maintains the stride-stance position described in Figure 5a- b. The therapist stands lateral to the patient’s lower extremity and then places his/her heel of the hand on the dorsal and distal tibial malleolus. This hand directs a force to the dorsal and distal tibial malleolus in a ventral direction as is indicated by the arrow above. At the same time the therapist’s cranial hand wraps medially around the patient’s leg and grabs the dorsal proximal gastrocnemius. With this hand the therapist simultaneously generates a spin force to the tibia into an externally rotated position. Please refer to Figure 6a above.

Figure 6b.
In order to improve ankle dorsiflexion in the closed chain the patient maintains the stride-stance position described in Figure 5a- b. The therapist stands medial to the patient’s lower extremity and then places his/her heel of the hand on the dorsal and distal fibular malleolus. This hand directs a force to the dorsal and distal fibular malleolus in a 30° ventral-lateral direction as is indicated by the arrow above. At the same time the therapist’s cranial hand wraps laterally around the patient’s leg and grabs the dorsal proximal gastrocnemius. With this hand the therapist simultaneously generates a spin force to the tibia into an internally rotated position. Please refer to Figure 6b above.
