Satpute K, Hall T, Bisen R, Lokhande P. Archives of Physical Medicine and Rehabilitation 2019;100:828-36.
Abstracted by Kasey Miller PT, DPT, COMT Kansas City, Missouri – Fellowship Candidate, IAOM-US Fellowship Program & Jean-Michel Brismée, PT, ScD, Fellowship Director, IAOM-US Fellowship program
Research: Evaluate the effect of spinal mobilization with leg movement (SMWLM) on low back and leg pain intensity, disability, pain centralization, and patient satisfaction in participants with lumbar radiculopathy.
Methods: A total of sixty participants (35 women) participated in this double-blind randomized controlled trial design. The participants were included if they had leg pain for greater than 6 weeks and evaluated for the presence of lumbar radiculopathy and displayed increased straight leg raise (SLR) range of motion (ROM) after a single trial application of SMWLM technique (Figure 1). The investigators also looked at reproduction of symptoms with straight leg raise (SLR) and tenderness on palpation of sciatic, tibial, or common peroneal nerves. Participants were excluded if they were not aged 18-60 years, if they had associated abnormalities of bowel and bladder function, lower extremity vascular disease, or physiotherapy/surgery for leg pain within 6 months. Participants were randomly allocated to either a SWMLM group or a control group. The SWMLM group received the mobilization, structured exercise, and transcutaneous electrical nerve stimulation (TENS). The control group only received structured exercise (Figure 2) and TENS. They did not receive the mobilization. Each group underwent six 50-minute treatment sessions carried out over 2 consecutive weeks. The primary outcome measurements were leg pain intensity and Oswestry Disability Index (ODI) score. Secondary variables were low back pain intensity, global rating of change (GROC), straight leg raise (SLR), and lumbar ROM. These variables were evaluated at baseline, post-intervention, and at 3- and 6-month follow-up.
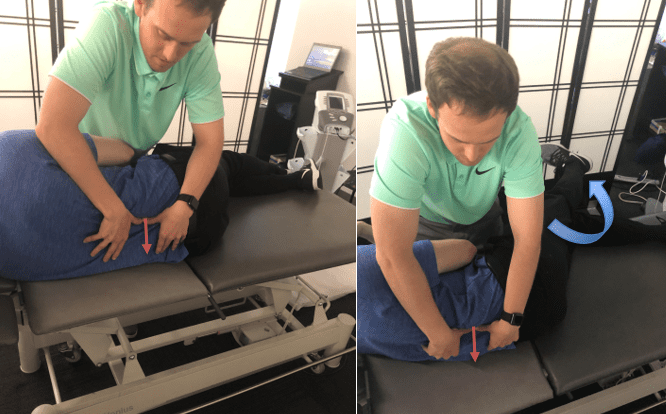
Figure 1: For the SMLWM, the therapist applied a firm transverse pressure to the superior vertebrae at the affected spinal level (left). At the same time, the participants were asked to move their affected leg to the limit of pain-free range of straight leg raise (right).

Figure 2: Structured exercise was described as performing 2 sets of 5-7 repetitions of lumbar spine ROM exercises in 4-point kneeling, comprising pelvic tilting and heel sitting (lumbar flexion).
Results: Significant and clinically meaningful improvement occurred in both primary outcome measures (Leg pain intensity and ODI score). At 2 weeks the SMWLM group had significantly greater improvement than the control group in leg pain (Mean Difference (MD) 2.0; 95% confidence interval (CI), 1.4-2.6) and disability via ODI score (MD 3.9; 95% CI, 5.5-2.2). Similarly, at 6 months, the SMWLM group had significantly greater improvement than the control group in leg pain (MD 2.6; 95% CI, 1.9- 3.2) and disability (MD 4.7; 95% CI, 6.3-3.1). The SMWLM group also reported clinically meaningful improvement in the secondary outcome measures (GROC, passive SLR, active lumbar flexion ROM, and area of limb pain).
Conclusions: The authors concluded the addition of SMWLM to a program, which consisted of exercise, and TENS provided significantly improved benefits in leg and back pain when treating patients with subacute lumbar radiculopathy. These benefits included reduction of leg and back pain, decreased disability via ODI, SLR ROM, as well as patient satisfaction in the short and long terms (6-month).
IAOM-US comments: Lumbar mobilizations are a readily applied treatment to those patients suffering from low back pain and radicular symptoms. However, there may be a more specific approach than the mobilization that was used in this study. Instead of simply applying a firm transverse pressure to the superior vertebrae at the affected spinal level, the IAOM-US suggests flexion/extension mobilizations that respect the lumbar spine biomechanics and anatomy. But before performing these techniques, it is important to identify the true pain generator, as this will dictate technique selection. There are several structures that can cause low back and leg pain. And all these structures have specific patterns that help clinicians identify the pain generator. For example, if the intervertebral disc is the pain generator the patient can display increased lumbar pain with sagittal motions (flexion/extension), increased pain with sitting, and a positive straight leg raise test.1,2 And if facet joints cause the low back pain, patients report increased pain with 3-dimensional quadrant testing and most likely increased pain with prolonged standing.3 Commonly associated with facet joint arthropathy is nerve root compression syndrome due to the hypertrophy of the facet joint narrowing the foramen space, impinging the nerve. Once clinicians have identified the pain generator they will be able to decide which technique is most appropriate for pain relief and improved function. Disc pathologies with radicular symptoms typically respond very well to axial separation (Figure 3) while facet pathologies and associated nerve root compression syndrome do well with joint specific traction (Figure 4) and flexion/extension mobilizations (Figures 5 and 6).4 While this study simultaneously performs the spinal mobilization and neural tissue mobilizations, the flexion/extension mobilizations that the IAOM-US utilizes may be better suited to be combined with neural tissue mobilizations than the spinal mobilization with leg movement, proposed by Mulligan.5 With the IAOM-US techniques, the biomechanics and anatomical features are respected by utilizing coupled and combined lumbar spine motions.6 If during the clinical exam clinicians discover the disc is the pain generator, axial separation will usually be a choice of treatment.4 However, if nerve roots are the pain generator, flexion mobilizations seem most effective as they open the foramen and reduce radicular symptoms.4 In the lumbar spine, the coupled motion in flexion is ipsilateral.7 With this knowledge, the IAOM proposes that the clinician pre-positions the patient in a side-lying manner with the painful side up and then ensures the affected segment is coupled. Once the clinician is positioned with the painful side up, the next step is to flex the affected segment. Before the clinician applies the mobilization force (from ASIS toward ischial tuberosity), coupled rotation can be added by rotating their top arm toward the ground. These steps ensure that the lumbar spine is coupled and the caudal vertebrae glide freely under the cranial vertebrae. Although the results of this study showed clinical significance using SMWLM combined with neural mobilizations, the IAOM-US proposes the pain generator guides the clinician’s decision about treatment technique selection. And choosing a more specific treatment can enhance treatment outcomes.

Figure 3: Axial separation is a direct technique for disc related symptoms. Midline pain with associated radicular symptoms as well as unilateral pain with no radicular symptoms can all indicate disc related symptoms.
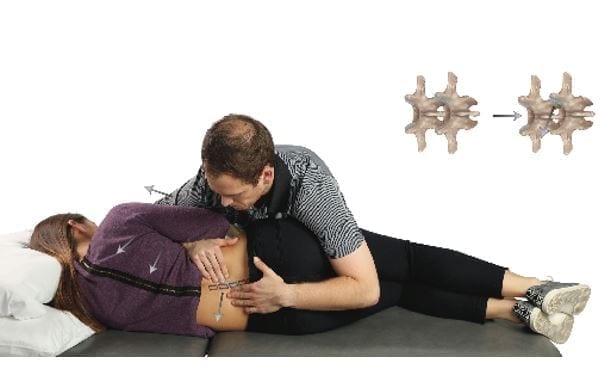
Figure 4: Joint Specific Traction (JST) is a great technique for pain dominant facet arthropathy. It can also be used as a warm up technique before performing flexion/extension mobilizations.

Figure 5: Flexion Mobilizations are performed by pulling in a line from the ASIS toward the ischial tuberosity. This particular technique is helpful for elderly patients with stenosis as well as those with difficulties bending over to tie their shoes.
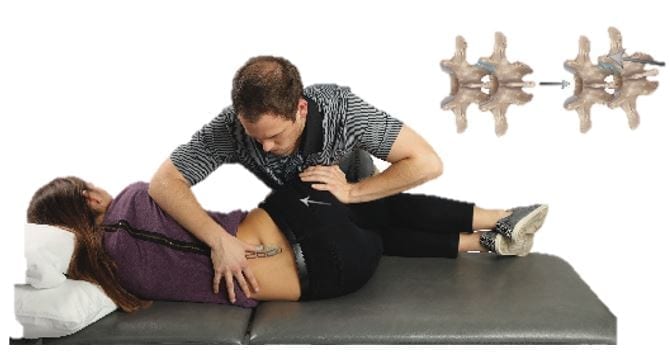
Figure 6: Extension Mobilizations are performed by pushing the ischial tuberosity toward the ASIS to initiate an extension moment of the caudal articulating process. This particular technique is helpful for those patients with difficulties standing upright. This is also a good technique for patients with stenosis but to make sure the technique is performed on levels above and below the stenotic segment.
References:
- Wilke H et al. New in vivo measurements of pressures in the intervertebral discs in daily life. 1999; 24:755-762.
- Ohnmeiss DD et al. Relation between pain location and disc pathology: A study of pain drawings and CT/discography. Clin J Pain. 1999; 15: 210-217.
- Revel M, Poiraudeau S, Auleley GR, Denke A, Nguyen M, Chevrot A, Germanian J: Capacity of the clinical picture to characterize low back pain relieved by facet joint anesthesia. Proposed criteria to identify patients with painful facet joints. 1998, 23: 1972-1977.
- Winkel D, et al. Diagonis and Treatment of the Spine. Aspen Publication; 1996.
- Mulligan BR, Manual Therapy: “NAGS,” “SNAGS,” “MWMS” etc. Wellington, New: Zealand: Plane View Services LTD; 2010.
- Cook C. Coupling Behavior of the Lumbar Spine: A Literature Review. J Man Manip Ther. 2003; 11(3); 137-145.
- Harrison D, Harrison D, Troyanovich S. Three-dimensional spinal coupling mechanics: Part one. J Manipulative Physiol Ther. 1998; 21: 101-113.
