Lantz JM, Emerson-Kavchak AJ, Mischke JJ, Courtney CA (2016). The International Journal of Sports Physical Therapy; 11(3): 450-461.
Summarized by: Courtney Van Dreese SPT, Missouri State University, Springfield, MO
Background: Patellofemoral pain syndrome (PFPS) is an overuse musculoskeletal disorder commonly diagnosed in the adolescent and young adult population with characteristic pain in the anterior or retro-patellar region of the knee. (Australian Group Musculoskeletal Pain Guidelines Group, 2003). Individuals with PFPS often experience an increase in pain with prolonged sitting (“theater sign”), deep squats, stair climbing, and kneeling. Due to the high variability of musculoskeletal disorders that can present as anterior knee pain, clinical diagnosis of PFPS is often one of exclusion (Clijsen et al., 2014). In physical therapy today, management of PFPS typically includes therapeutic exercise (specifically quad strengthening) and realignment procedures incorporating taping, bracing, and orthotics (Crossley et al., 2002). Without management of acute pain symptoms, musculoskeletal injury such as PFPS may evolve into a more chronic presentation. As the research has shown, chronic musculoskeletal issues can result in a state of persistent pain. This state is characterized by increased CNS signals causing hypersensitivity and central sensitization (Winkelstein, 2004).
Research: The purpose of this case study is to present the clinical findings and success in treating an individual with chronic PFPS utilizing tibiofemoral joint mobilization as part of the treatment regimen. Specifically, this case report discusses the effects that tibiofemoral joint mobilization has on patient pain, function, and central processing of pain.
Details of Paper: A 28-year-old female presenting with a two year history of left anterior knee pain was referred to physical therapy for conservative treatment per her sports medicine physician. This was her second time trying physical therapy, with failed outcomes at restoring her functional level twenty months prior. An MRI showed no significant findings in the joint.
The patient presented initially with anterior knee pain that would radiate into the posterior knee and anterior lower leg after activities including stair climbing, squatting, kneeling, and prolonged sitting. Relief of pain came from medications and frequent sitting breaks. The patient stated her primary goal was to return to an independent level of functioning including the ability to dance, exercise, and walk long distances without pain.
There is ample evidence supporting the researcher’s suspicion of central sensitization in this case including a two year history and chronicity of symptoms, complaints of knee instability, a previous failed physical therapy attempt, cold thermal hypersensitivity, and reported outside events causing the patient emotional stress.
Upon initial examination, the patient displayed poor posture overall, an antalgic gait pattern, palpation tenderness and allodynia (pain did not follow a dermatomal pattern), hip/quadricep weakness and lower extremity biomechanical abnormalities (left dynamic medial collapse). Upon joint-specific testing at the hip, knee, and ankle, the only arthrokinematic motion to reproduce the patient’s anterior knee pain was tibiofemoral posterior-anterior translation at approximately fifty percent of the joint resistance.
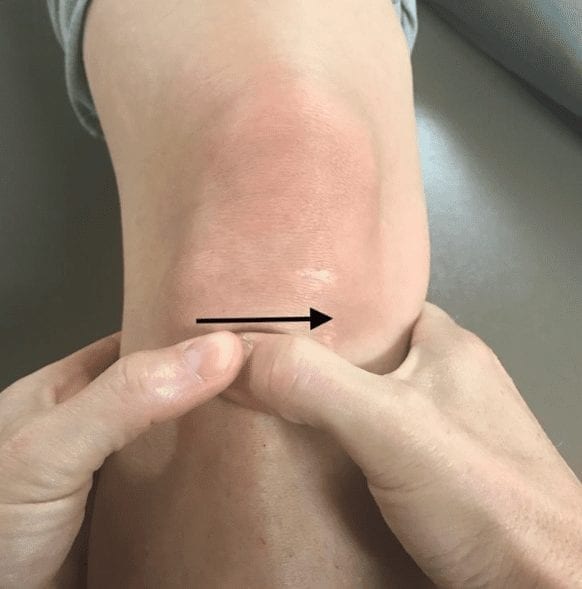
Intervention: The patient in this case report attended nine total physical therapy sessions. At the initial evaluation, multiple outcome assessments (described in the next section) were used as pre-assessment measures. At the first five visits, treatment consisted of grade III tibiofemoral posterior-anterior joint mobilizations only. The specific technique for this mobilization is displayed in Figure 1 and described below it. During this time, the patient was also instructed to complete a home exercise program (HEP) involving therapeutic exercise and neuromuscular re-reeducation to target abnormal joint mechanics. Visit six utilized grade III anterior-posterior joint mobilization at the talocrural joint bilaterally to treat hypomobility (no pain) found during the initial examination. The final three sessions did not involve joint mobilization and focused on balance training for additional neuromuscular reeducation, along with an accompanying HEP.
Outcome Measure(s): There were a multitude of outcome measures used in this study to further provide evidence of successful treatment. Subjective outcomes were assessed using the Kujala Anterior Knee Pain Scale (Kujala Scale), Numeric Pain Rating Scale (NPRS), Global Rating of Change (GROC), and the Fear-Avoidance-Belief Questionarre (FABQ). Results of each assessment met the minimal clinically important difference (MCID) at discharge in comparison to scores at initial evaluation. Patient scores continued to progress two months post-treatment as recorded by phone call.
To determine changes in deep tissue sensitivity, a Pressure Pain Threshold (PPT) was measured one centimeter below the patella (most painful spot per subjective reporting from patient). The patient was able to increase her PPT from 119kPa at initial evaluation to 386 kPa at discharge, indicating decreased active nociceptive pathways and movement away from the chronic pain cycle.
The Step Down Test was utilized to assess functional performance of the patient with the addition of the NPRS after testing for subjective pain complaints. Results of this case study showed an increase in score from 11 steps at initial evaluation to 40 steps at discharge, demonstrating improved functional ability of the patient.
Clinical Impression: This article highlights the possible significant value in the addition of joint mobilizations (specifically tibiofemoral) when treating patients with chronic PFPS to target the centrally-mediated pain component. Since this patient presented with allodynia of the anterior knee and decreased PPT, a component of her pain is likely centrally-mediated indicating hyperactivity of CNS nociception pathways. Looking at the biomechanics of the joint itself, posterior translation of the tibia on the femur creates a position of knee flexion, which also increases patellofemoral compression. It is important to note that joint mobilization alone will not produce desired outcomes, as this study demonstrated the additional use of therapeutic exercise and neuromuscular re-education in restoring joint mechanics. Currently, there is no single approach in the treatment of PFPS that is deemed most beneficial due to its multifactorial nature (Wilk et al., 2001).
Conclusions: This case study may possibly suggest that mobilization at the tibiofemoral joint might be considered for patients presenting with chronic PFPS, specifically due to its ability in decreasing active nociceptive pathways and eliminating central sensitization of pain.
Personal Commentary: As previously stated, the etiology of PFPS is currently unknown and difficult to assess in the clinic. For these reasons PFPS is a diagnosis I would like to become more confident in evaluating and treating. As a student, I had not yet considered using tibiofemoral joint mobilizations to target the centrally-mediated pain component in chronic PFPS cases until reviewing this study. Further, I was not aware that central sensitization may exist with patellofemoral pain since most research does not discuss this factor. In my opinion, this study discusses a technique that may help guide our future treatment of chronic PFPS.
As the profession of physical therapy is still working towards country-wide direct assess in patient care, this keeps the likelihood of evaluating patients in a state of chronic pain high. Have clinicians successfully treated patients with PFPS in the past, only to find that patient returning for treatment years later? Our treatment of musculoskeletal dysfunction must address this chronic pain component if we want successful outcomes that last.
According to an article by Ivković, et al. (2007), PFPS is one of the most common sports-related injuries in females next to stress fractures and lateral epicondylitis. Further, PFPS was noted in 20% of females compared to only 7.4% of males (Ivkovic et al., 2007). As a former division one collegiate athlete, I have struggled with patellofemoral pain for quite some time now without significant long-term benefit of therapeutic exercise alone. Knowing now that PFPS can easily become a chronic issue suggests that tibiofemoral joint mobilizations may be of benefit. At my future clinical internships and as a practicing clinician, I will be sure to employ these principles in my patient care and assess for components of chronic pain as this could facilitate long-term success in patient function.
References:
Australian Acute Musculoskeletal Pain Guidelines Group (2003). Evidence-based management of acute musculoskeletal pain. Australian Academic Press Pty. Ltd. [PDF]
Clijsen, R., Fuchs, J., & Taeymans, J. (2014). Effectiveness of exercise therapy in treatment of patients with patellofemoral pain syndrome: systematic review and meta-analysis. Physical Therapy, 94(12). 1697-1708.
Crossley, K., Bennell, K., Green, S., Cowan, S., & McConnell, J. (2002). Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo controlled trial. The American Journal of Sports Medicine, 30(6). 857-865. doi: 10.1177/03635465020300061701
Ivković, A., Franić, M., Bojanić, I., & Pećina, M. (2007). Overuse injuries in female athletes. Croatian Medical Journal, 48(6), 767–778. doi:10.3325/cmj.2007.6.767
Wilk, K.E. & Reinold, M. M. (2001). Principles of patellofemoral rehabilitation. Sports Medicine and Arthroscopy Review, 9. 325-336
Winkelstein, B.A. (2004). Mechanisms of central sensitization, neuroimmunology and injury biomechanics in persistent pain: implications for musculoskeletal disorders. Journal of Electromyography and Kinesiology, 14(1). 87-93.